Are you aware that different meals need different strategies when it comes to timing your insulin? Depending on the macronutrient breakdown of the meal: high in fat or protein, low in carbohydrates, or a balance with moderate amounts of each, you want to take your insulin in a way that matches the digestion of the meal so that you can keep those blood sugars in range. The carbohydrate count is not the only thing that you want to be paying attention to! Learn how to Take Insulin for Different Types of Meals.
Note that each person is individual and the type of insulin you have access to (rapid or regular) would change your technique. Some insulins work faster than others. But let’s talk about some strategies you need to consider when getting started.
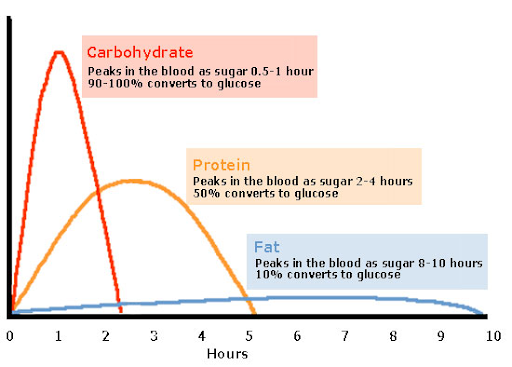
First, let’s ‘mind our macronutrients’. Here is a great visual showing how long it takes for carbohydrates, protein, and fat to digest:
So the next question is, what happens when we combine these macros all together at a meal in different proportions?
The Balanced Meal
Let’s start with the simplest meal to dose insulin for. Think of the ‘balanced meal’ as one with some carbohydrate (minimum 15+ g), moderate protein (palm size or 3oz) and minimal fat. For most people on rapid types of insulin, taking their insulin for the meal 15-20 minutes in advance (pre-bolus) will match the glucose curve. So, how to take Insulin for Different Types of Meals?
High Protein, Low or No Carbohydrate
Have you ever eaten a “no carb” meal and noticed your blood sugar still went up afterward? Something like a salad with chicken breast perhaps? Part of the reason is that your liver will turn a portion of the protein you ate into glucose (via a process called gluconeogenesis) (1,2). This is much more noticeable when you eat much more protein than usual and/or you don’t eat any obvious carbs at the meal.
One study shows that, without carbs, at least 75g of protein needs to be eaten before an effect on blood sugar will be seen(6). On the other hand, the Fat Protein Unit method (FPU) recommends taking extra insulin for every 25 g of protein eaten (3). So, what on earth are we supposed to be doing with our insulin dosing?
What I have seen with my Type-1 patients (including myself) for low-carb meals is that protein eaten in absence of carbs, even if it is their usual portion of protein, needs to be covered with meal-time insulin.
The exact amount of protein that needs to be covered by insulin is thought to be roughly 20-50%, but again that varies from person to person (1, 4).
Taking your insulin after eating instead of before can also be helpful to prevent low blood sugar after the “no-carb” meal! But it depends on the type of insulin you use!
High fat meal, Includes Carbohydrates
If you look at the chart above, you will see that fat can affect your blood sugar for up to 10 hours after a meal. Fats slow down digestion, meaning blood sugar response will be delayed, taking 3-5 hours to be reflected in your blood sugar(2). Additionally, fat causes insulin resistance, meaning you need extra insulin on top of your carb count to cover the meal(5).
Think of foods like… pizza, nachos, and fettuccine alfredo.
If you take too much insulin up front there is a good chance you will have a low blood sugar with a rebound high blood sugar later on. To avoid this you want to split up the insulin dose, especially if you are using rapid types of insulin for your meals. If you wear an insulin pump you would want to use the ‘extend bolus’ feature, where the pump would slowly drip the insulin over a few hours instead of giving it all upfront as a regular bolus. Neat, right?
There are a couple of few different ways to account for the extra fat in a meal and add the extra insulin to cover the fat-related insulin resistance.
You may or may not have heard of the Warsaw Equation which uses “Fat Protein Units” (FPU’s) (3). This method tells you exactly how long to extend the bolus for, based on the amount of protein and fat in the meal.
I personally like to use a simpler method with my clients that uses a meal “factor” for higher-fat meals. Fat and protein units don’t need to be calculated. Insulin doses would only be calculated from the carb count, just like a balanced meal, and then the meal factor (aka “fat factor”) would be added onto it.
This still makes up for the added insulin resistance from the high-fat content, without having to do too much math. And as always with Type-1 Diabetes, it requires a bit of trial and error.
The key thing to remember is that if the insulin works faster than how quickly food/carbs are digested in your bloodstream, you are going to have low blood sugar within the first few hours of eating.
With any kind of meal, the goal is to match your insulin’s action time to the rate of digestion of your meal!
Important note: Each person living with Type-1 Diabetes is unique. They may be using different types of insulin, have different levels of insulin resistance and have different rates of digestion for meals. These are general principles I consider when guiding a client on how to “dose for their meals” with insulin. It is wise to consult your doctor or a Certified Diabetes Educator before becoming bold with your insulin.
Or Find me on Instagram @bolus.eat.live!
*limited time only
Maya Perko
My name is Maya, and I am a Registered Dietitian who also happens to be living with Type-1 Diabetes for the past 17 years. I have a passion for helping people living with diabetes find confidence balancing their blood sugars, so that they can handle anything life throws their way. In my free time I like to go hiking, rollerblading and travel (especially off the beaten path).




